Tangible Pain Assessment Tools
Tangible Pain Assessment Tools
Tangible Pain Assessment Tools
Role
Role
Undergraduate Thesis
Undergraduate Thesis
Services
Services
Product Design
Product Design
Industries
Industries
Health care
Health care
Duration
Duration
6 months
6 months
Tangible Pain Assessment Tools are expressive, tactile tools that help overcome a multitude of communication barriers so that children can self-report their pain adequately. By avoiding verbal expression, the purpose of TPAT is to develop a cross-cultural research tool to self-report pain.
Consultation and Guidance - Dr. Daniel Tsze, Columbia University Medical Center.
Tangible Pain Assessment Tools are expressive, tactile tools that help overcome a multitude of communication barriers so that children can self-report their pain adequately. By avoiding verbal expression, the purpose of TPAT is to develop a cross-cultural research tool to self-report pain.
Consultation and Guidance - Dr. Daniel Tsze, Columbia University Medical Center.
Current tools rely on culturally specific tropes: a 10-point scale on the one hand, and drawings of faces on the other.
Current tools rely on culturally specific tropes: a 10-point scale on the one hand, and drawings of faces on the other.
The Numerical and face-based scales (e.g. Wong-Baker Faces Pain Scale, Faces Pain Scale-Revised) are most commonly used to assess pain. The numeric pain scale is too simple, a rating of 4 to 7 is considered moderate. Mild pain is rated 1 to 3. Over 7 is considered severe (Neighmond, 2018). This leads the doctors to "treat by numbers.” If your doctor gets the wrong idea about your pain, it's not only going to affect your comfort — it can affect your treatment. If they just look at a number, they may be more likely to over-treat or prescribe more medication, which can be worrisome during an era of concern about opioid abuse and addiction.
Starting at age 3 or 4, children are asked to self-report their pain. The numerical and faces scales require a certain level of expressive capacity that younger children may not have and give no information regarding the character of pain that the child is experiencing. In addition, children may have a number of barriers that prevent accurate communication of their pain, ranging from cognitive impairments to developmental differences that make these scales inadequate for the task at hand. Doctors need to tailor assessment strategies to the child's developmental level – Strategies that involve their imaginations and sense of play.
By avoiding verbal expression, the purpose of TPAT is to develop a cross-cultural research tool to self-report pain.
The Numerical and face-based scales (e.g. Wong-Baker Faces Pain Scale, Faces Pain Scale-Revised) are most commonly used to assess pain. The numeric pain scale is too simple, a rating of 4 to 7 is considered moderate. Mild pain is rated 1 to 3. Over 7 is considered severe (Neighmond, 2018). This leads the doctors to "treat by numbers.” If your doctor gets the wrong idea about your pain, it's not only going to affect your comfort — it can affect your treatment. If they just look at a number, they may be more likely to over-treat or prescribe more medication, which can be worrisome during an era of concern about opioid abuse and addiction.
Starting at age 3 or 4, children are asked to self-report their pain. The numerical and faces scales require a certain level of expressive capacity that younger children may not have and give no information regarding the character of pain that the child is experiencing. In addition, children may have a number of barriers that prevent accurate communication of their pain, ranging from cognitive impairments to developmental differences that make these scales inadequate for the task at hand. Doctors need to tailor assessment strategies to the child's developmental level – Strategies that involve their imaginations and sense of play.
By avoiding verbal expression, the purpose of TPAT is to develop a cross-cultural research tool to self-report pain.

Research
Research
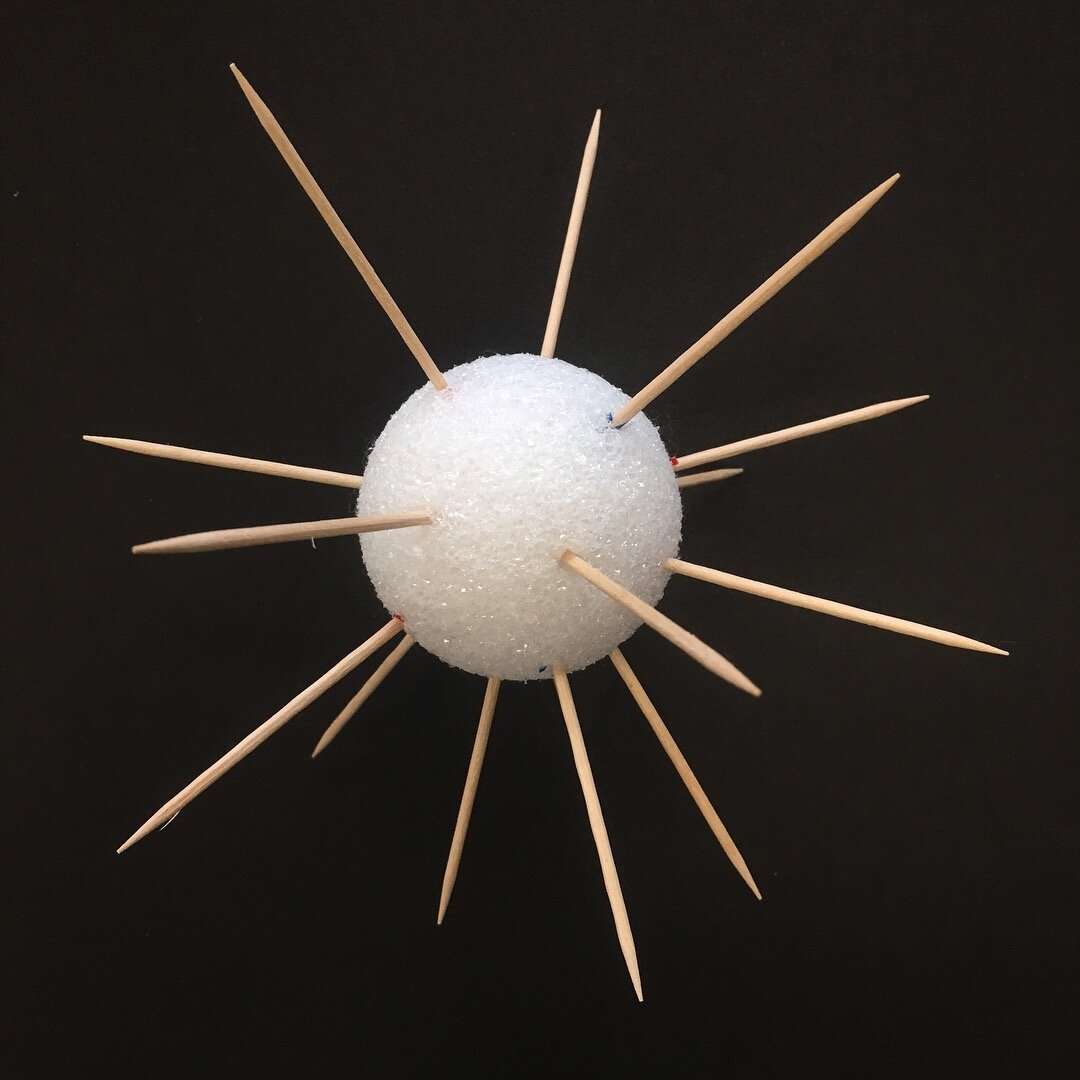
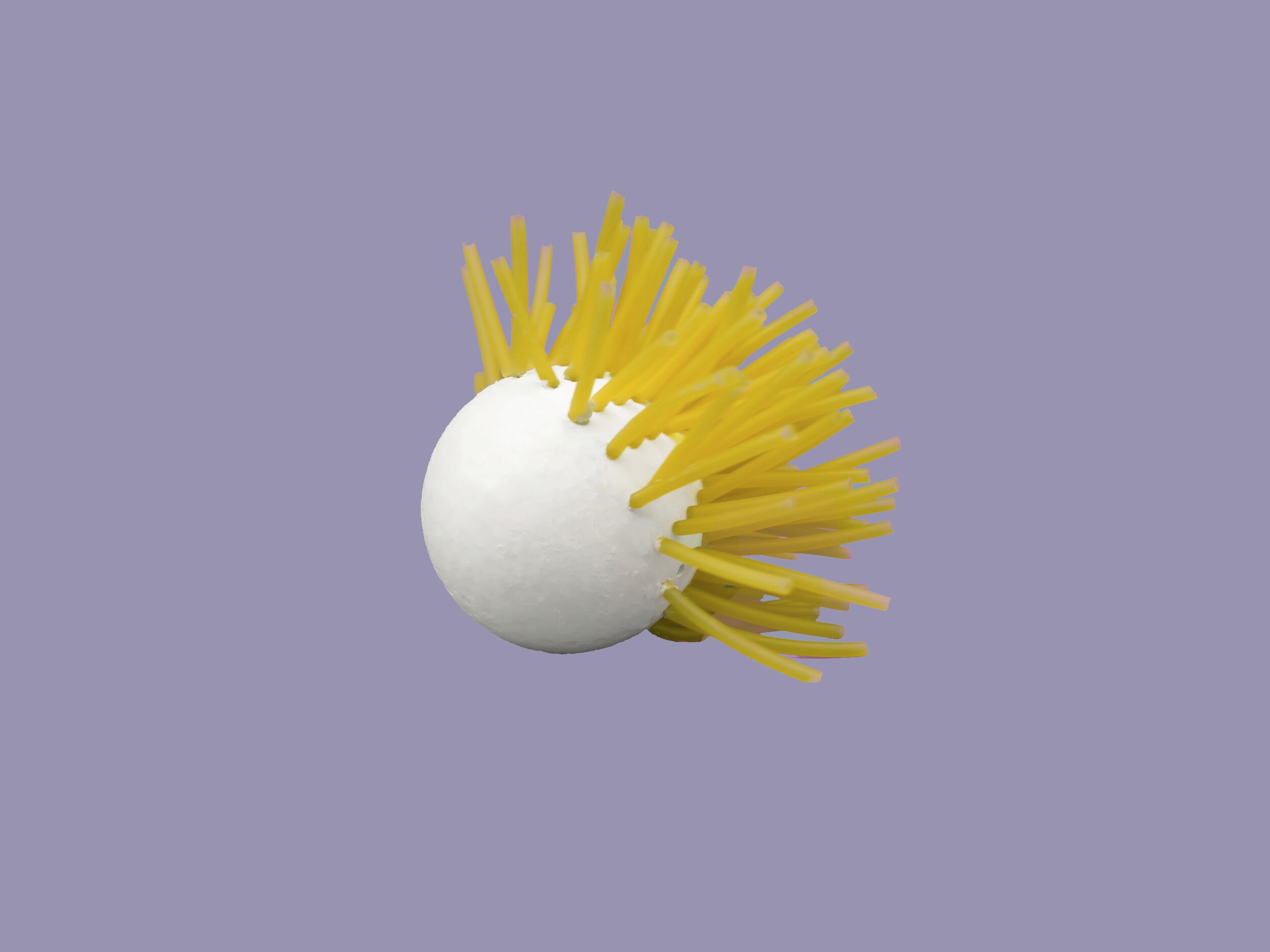
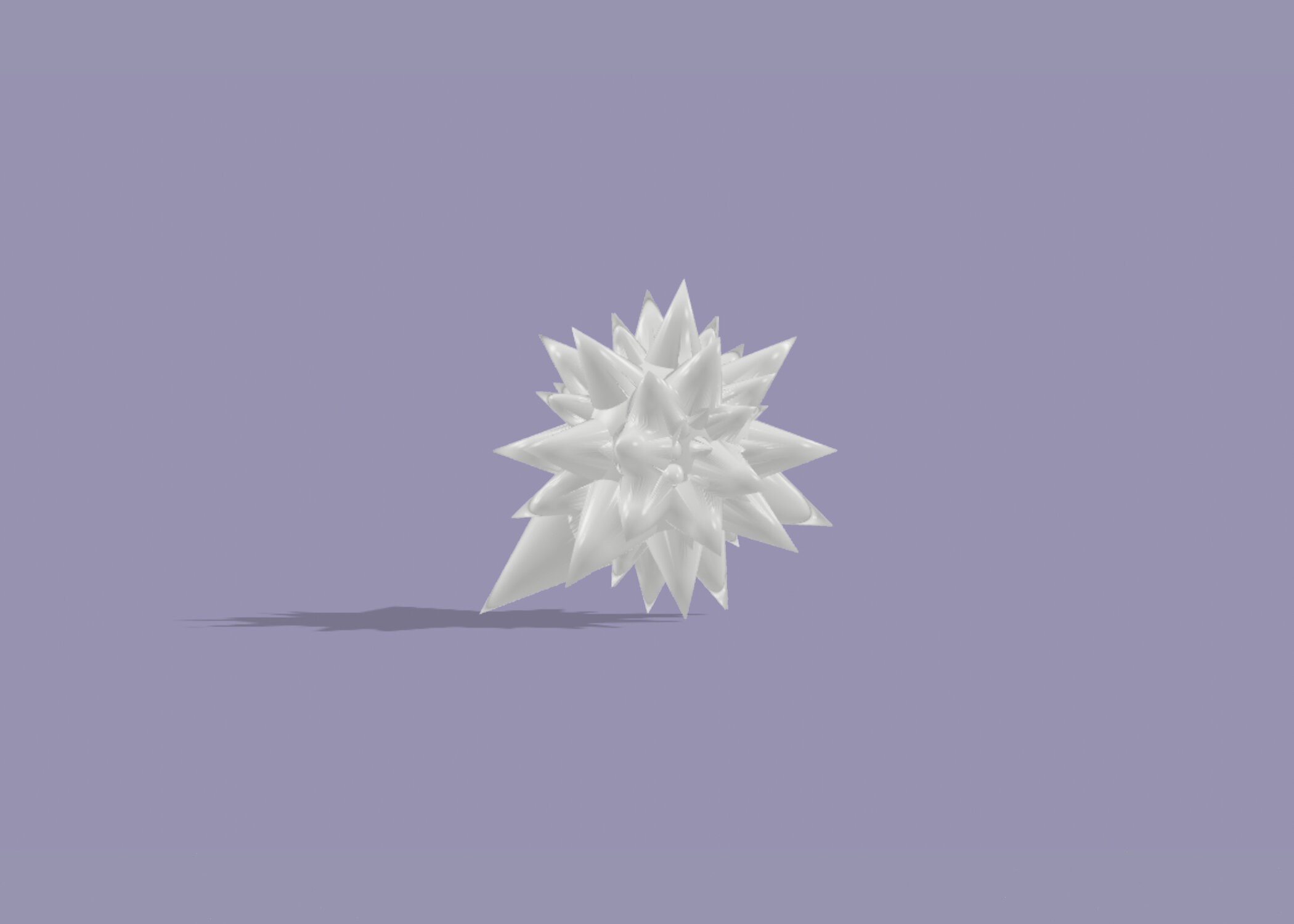
I started my research by asking adults and children to draw their experience of pain on a piece of paper. Adults drew cactus and a spiky ball but younger children struggled to communicate their pain. A 10-year-old girl drew a picture of a car because being in pain makes her feel nauseous and she gets motion sickness when she is in a car.
I reached out to pediatric emergency medicine physician and researcher Dr. Daniel Tsze from Columbia University Medical Center, who has done extensive research on the assessment and treatment of pain in children. We started prototyping different iterations of the objects using things found at a dollar store.
I started my research by asking adults and children to draw their experience of pain on a piece of paper. Adults drew cactus and a spiky ball but younger children struggled to communicate their pain. A 10-year-old girl drew a picture of a car because being in pain makes her feel nauseous and she gets motion sickness when she is in a car.
I reached out to pediatric emergency medicine physician and researcher Dr. Daniel Tsze from Columbia University Medical Center, who has done extensive research on the assessment and treatment of pain in children. We started prototyping different iterations of the objects using things found at a dollar store.




Continuous Assessment
Continuous Assessment
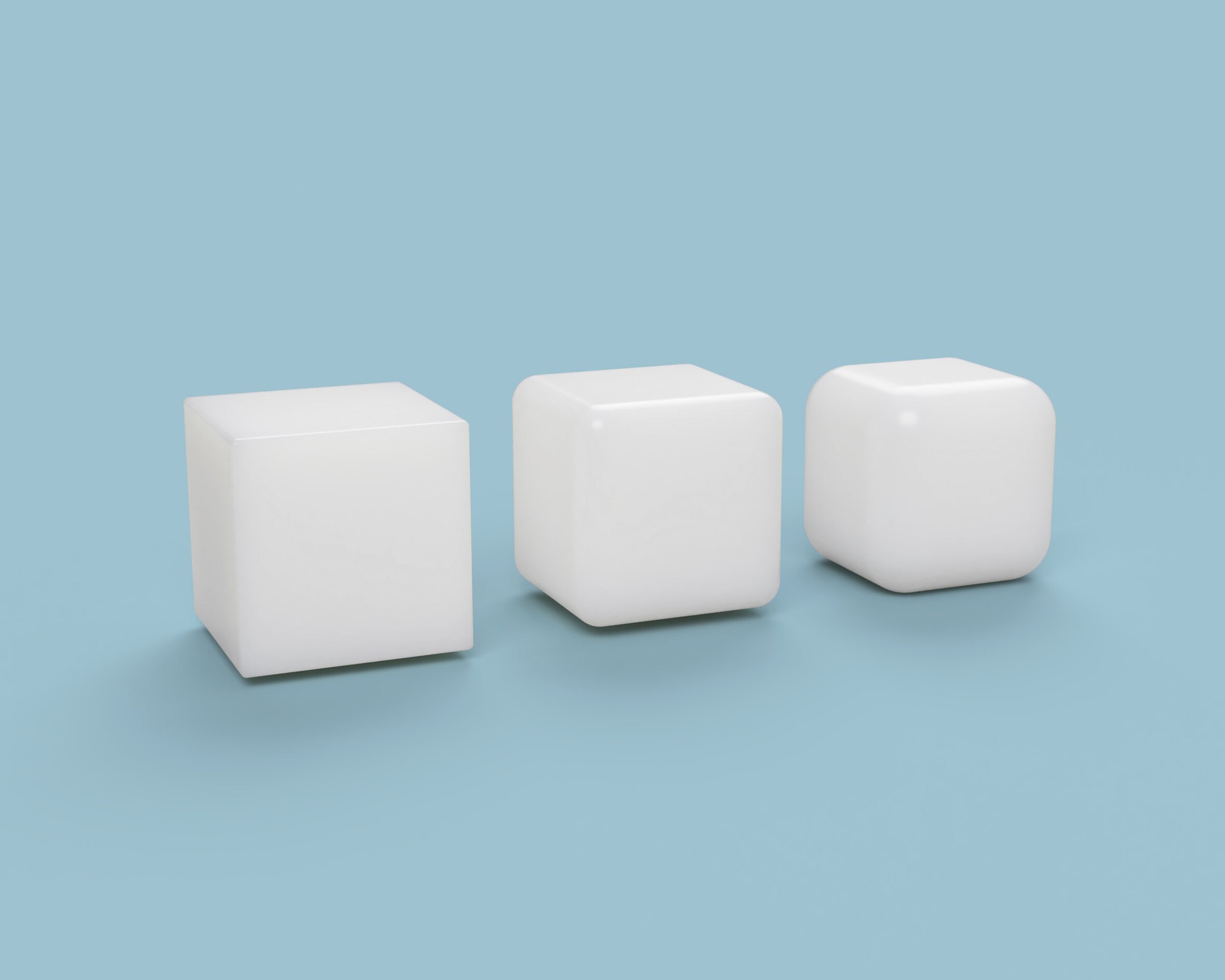
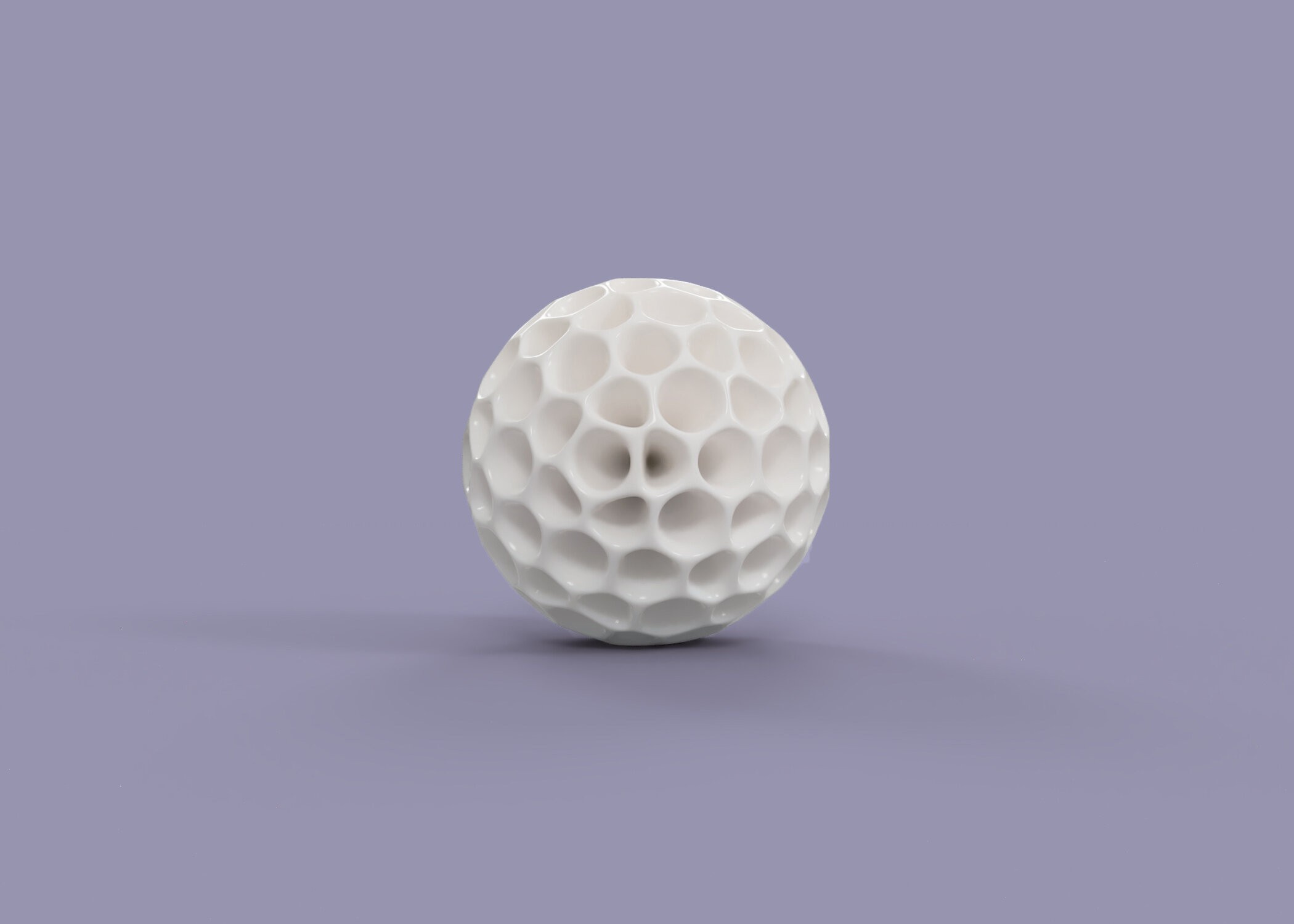
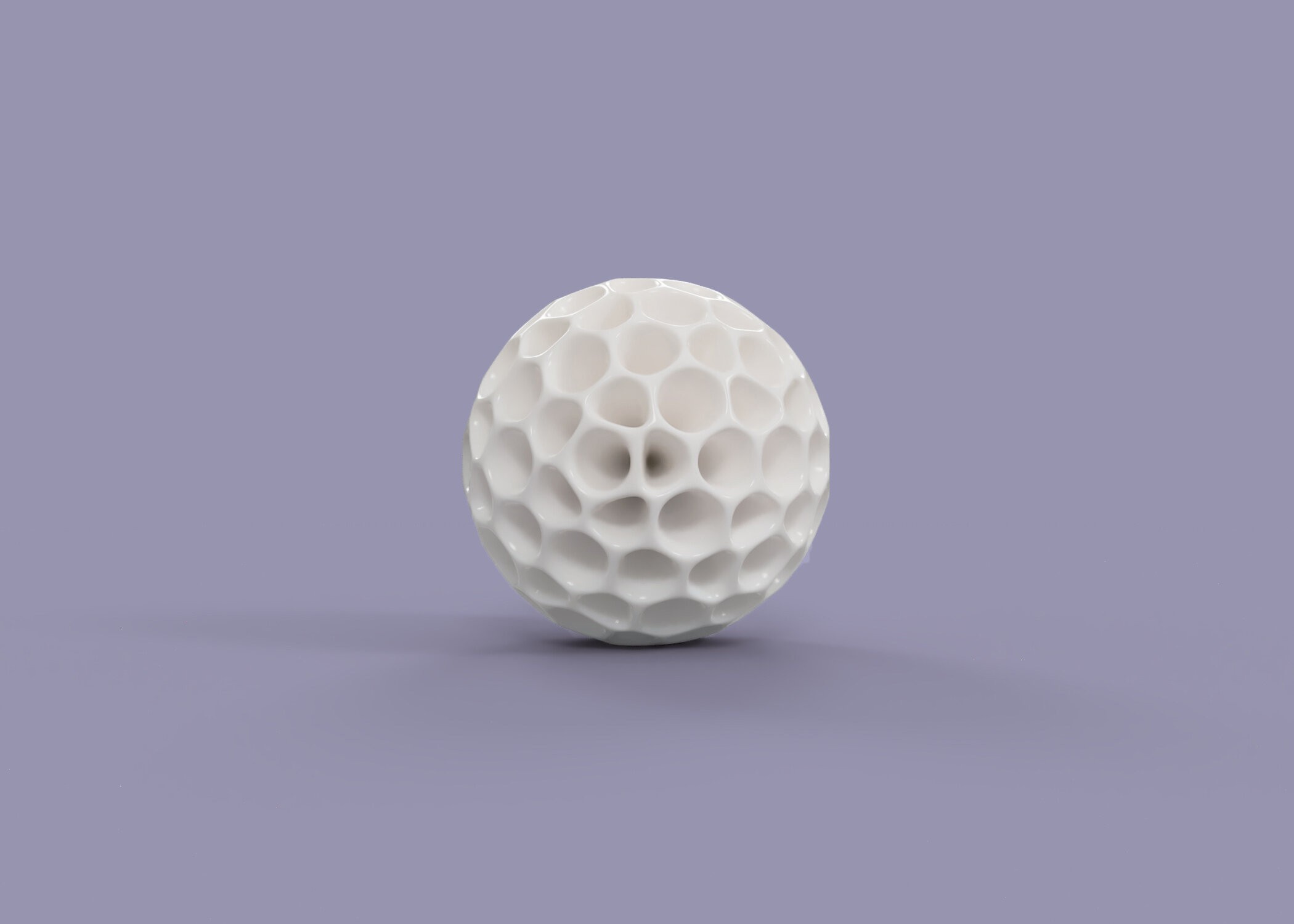
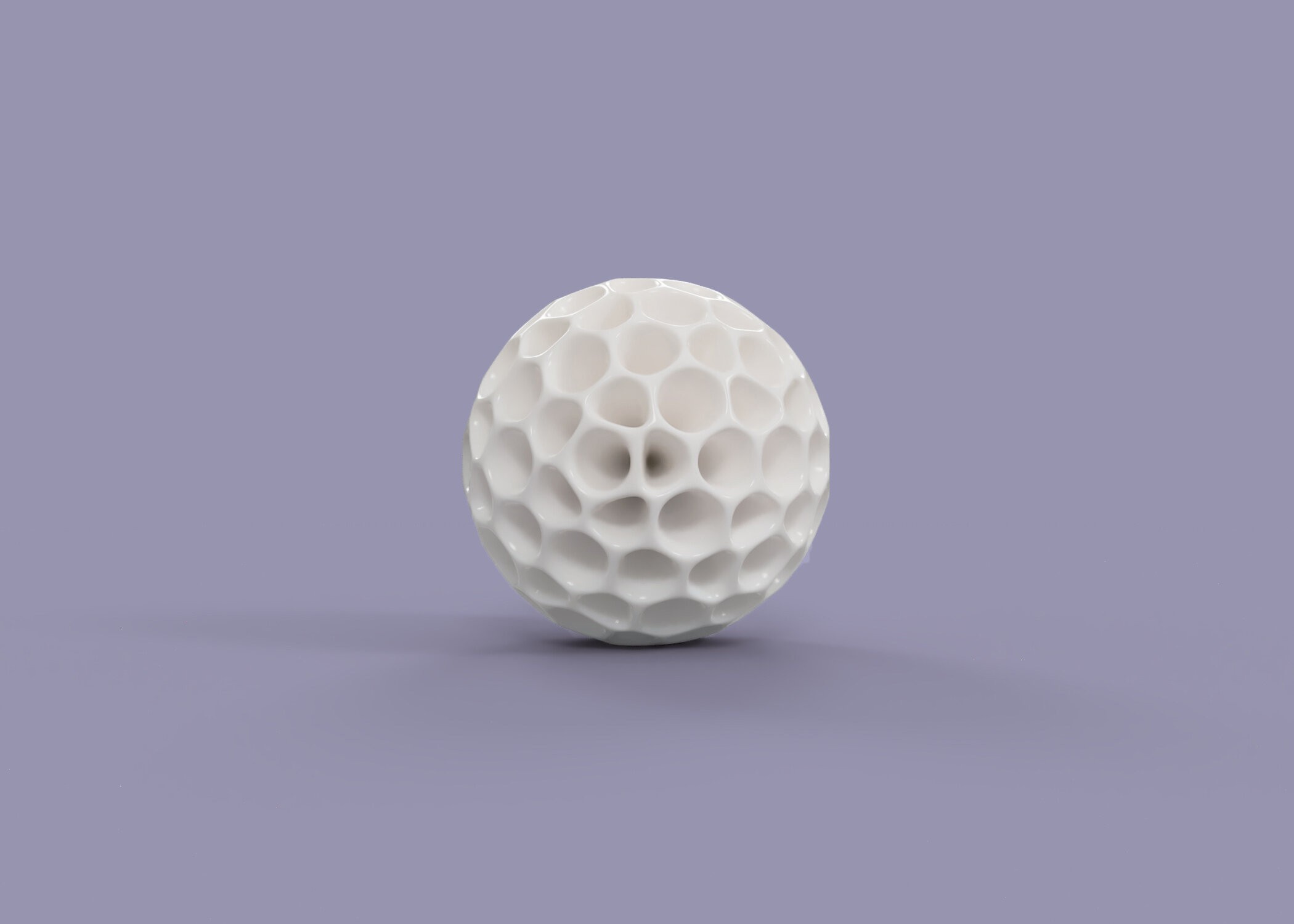
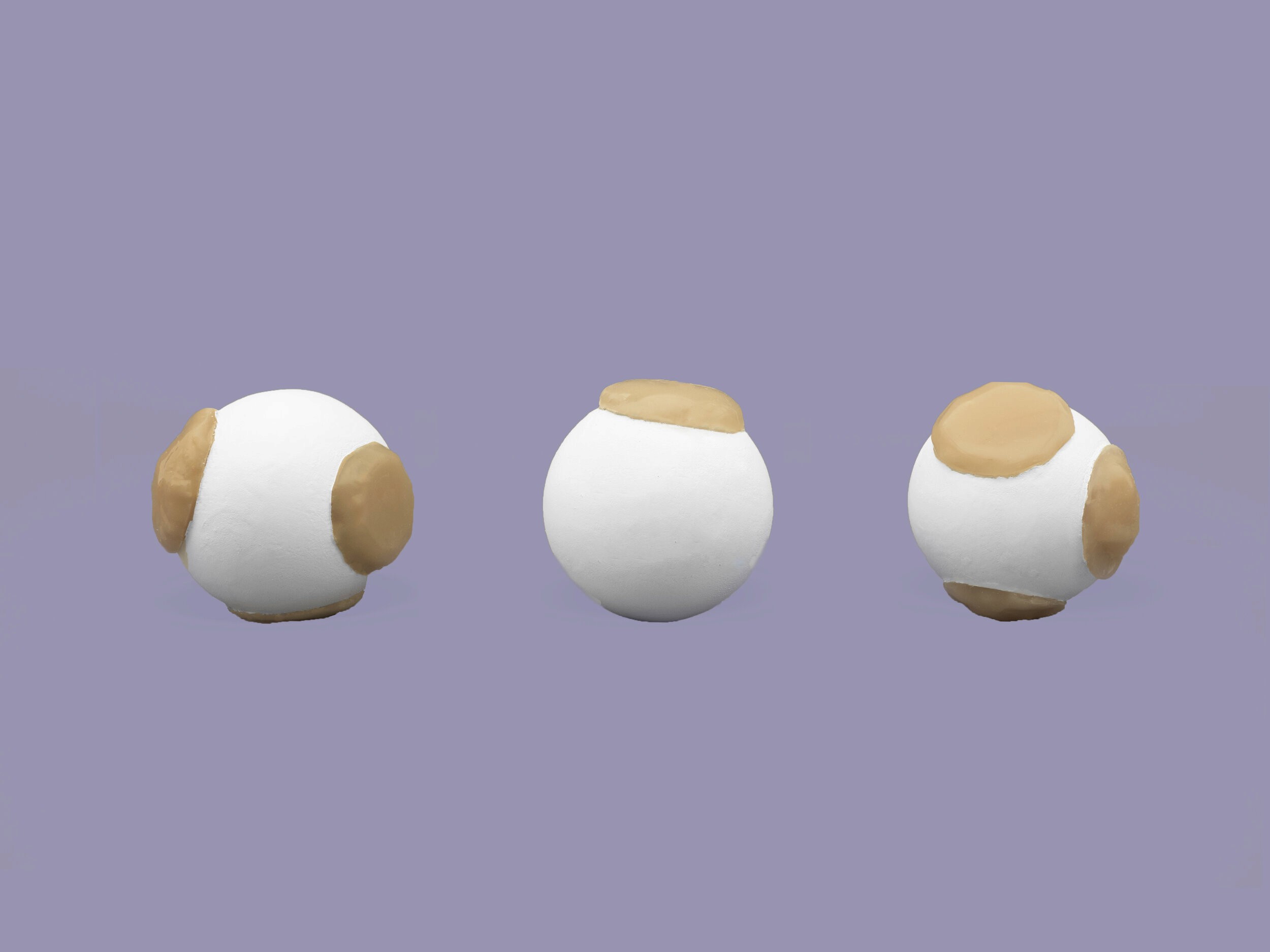
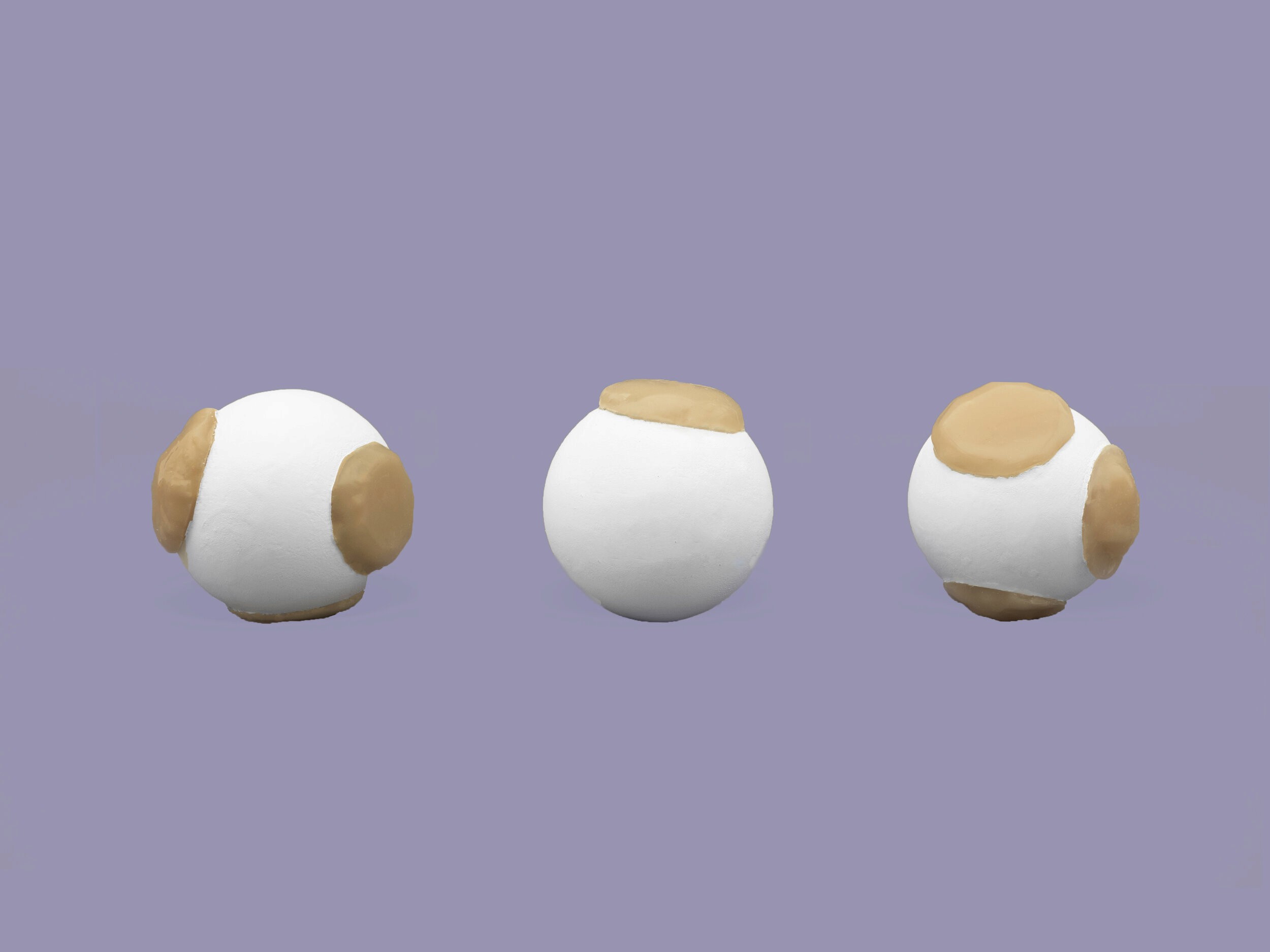
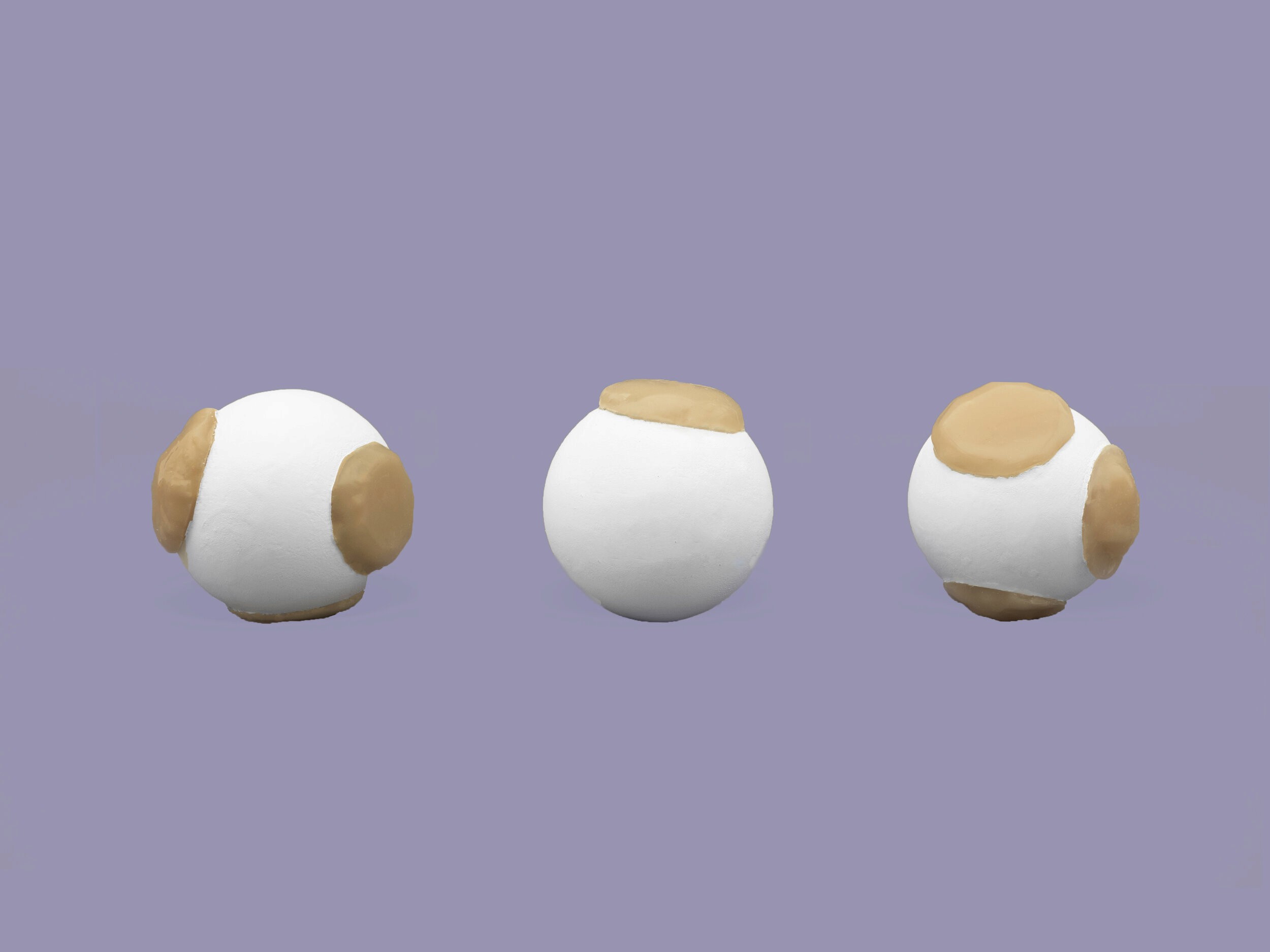
The first tool I developed was a continuous (quantitative) assessment scale. This tool helps describe the intensity of the pain. It is inspired by the Goldilocks principle, named by analogy to the children’s story, Goldilocks and the Three Bears. Goldilocks tastes three different bowls of porridge, and she finds that she prefers porridge which is neither too hot nor too cold but has just the right temperature. Since the concept of “just the right amount” is easily understood. The scale consists of three objects varying in size and roundness that describe the intensity of pain from low, medium to high. Instead of providing children with 10 response options which can be difficult to understand, they are provided with 3 response options that allow them to make their choice more decisively and efficiently. This is especially true with 3 to 4-year-olds, according to the research conducted by Dr. Carl Von Baeyer (Baeyer, 2017).
The first tool I developed was a continuous (quantitative) assessment scale. This tool helps describe the intensity of the pain. It is inspired by the Goldilocks principle, named by analogy to the children’s story, Goldilocks and the Three Bears. Goldilocks tastes three different bowls of porridge, and she finds that she prefers porridge which is neither too hot nor too cold but has just the right temperature. Since the concept of “just the right amount” is easily understood. The scale consists of three objects varying in size and roundness that describe the intensity of pain from low, medium to high. Instead of providing children with 10 response options which can be difficult to understand, they are provided with 3 response options that allow them to make their choice more decisively and efficiently. This is especially true with 3 to 4-year-olds, according to the research conducted by Dr. Carl Von Baeyer (Baeyer, 2017).
Categorical Assessment
Categorical Assessment
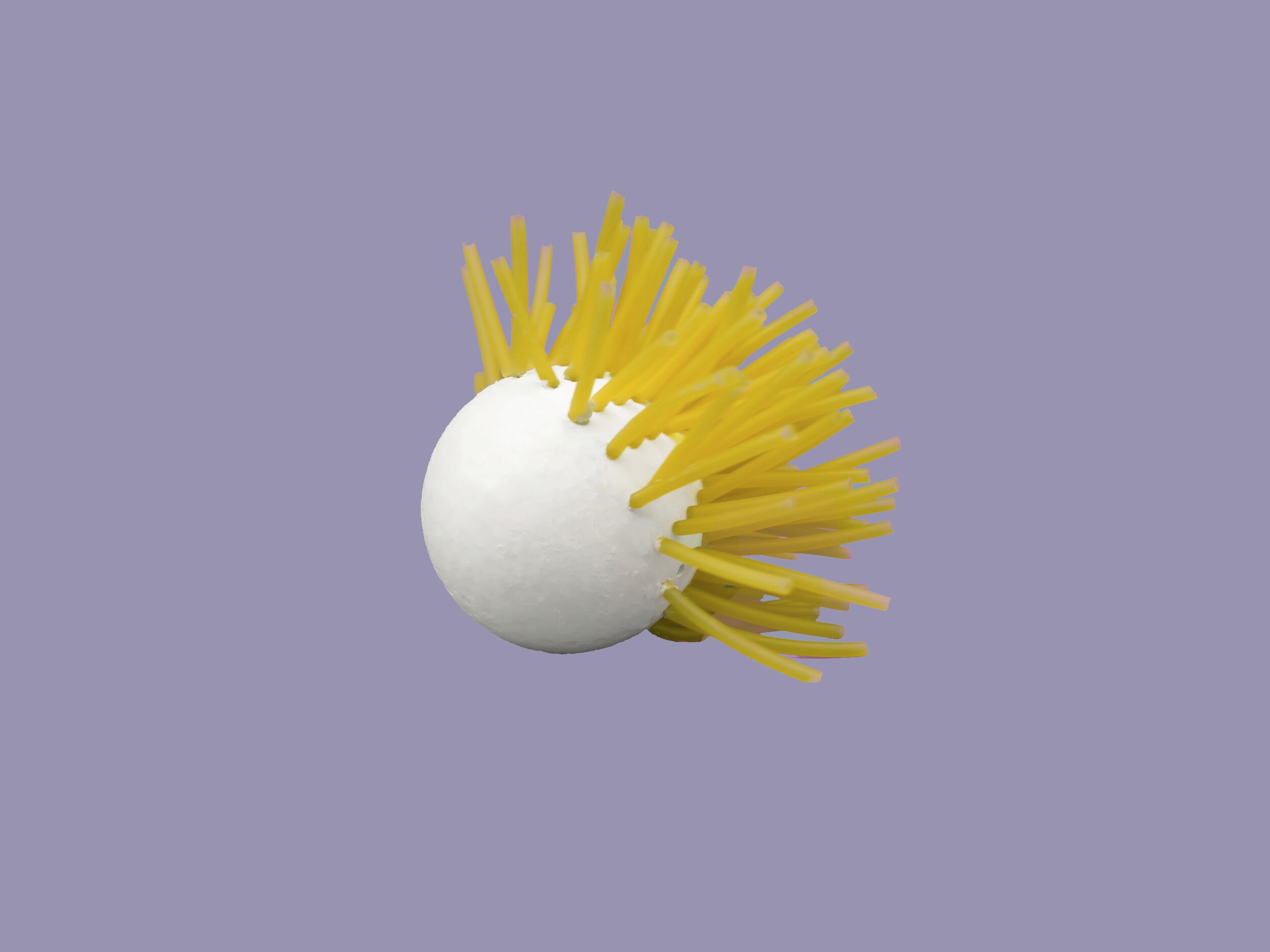
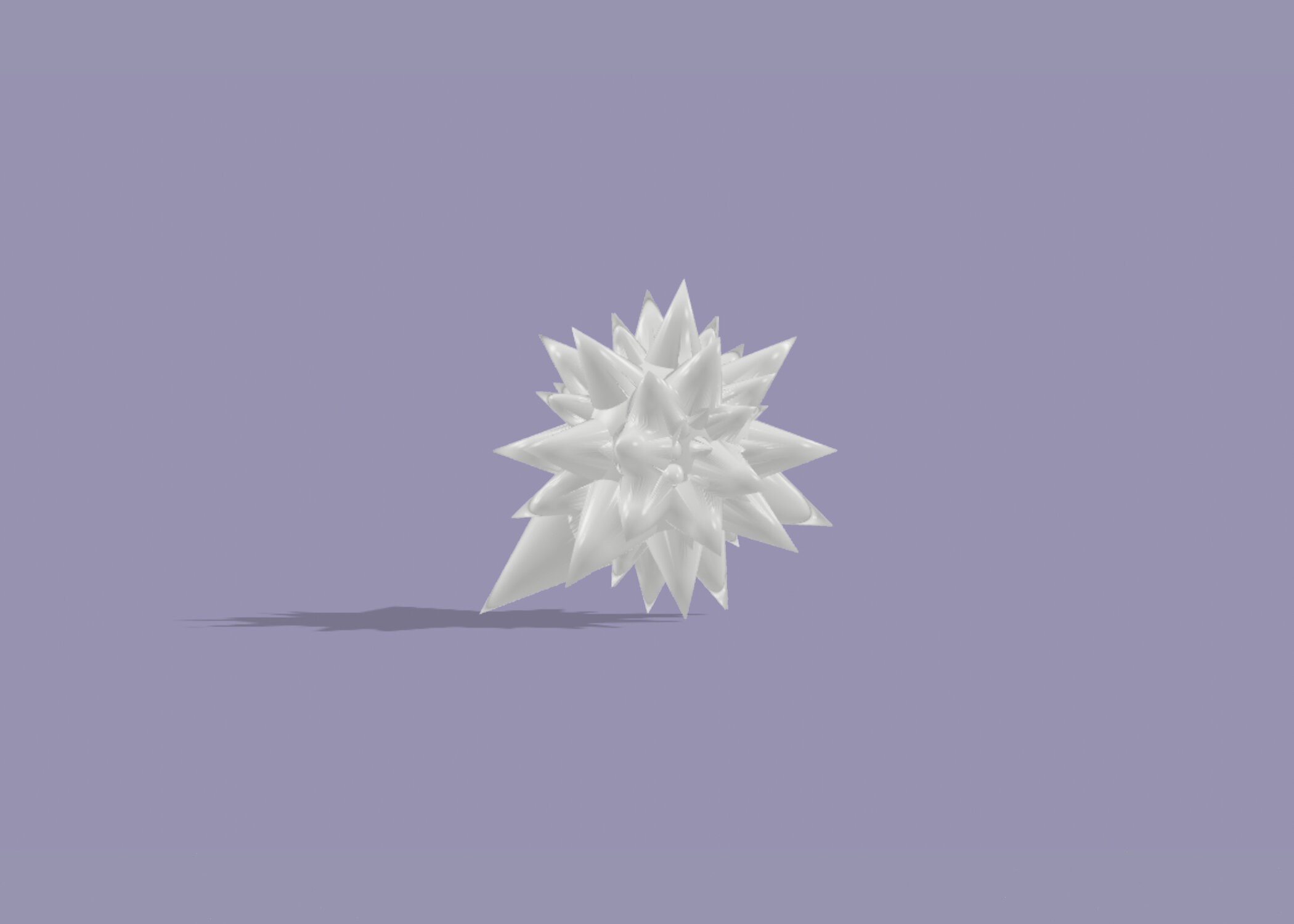
These tools help identify the character of pain (such as sharp or dull pain, soreness, stabbing, or throbbing pain) that clinicians rely on to make accurate diagnoses when children are unwell. They are tactile and offer a range of expressive possibilities, allowing young children to communicate qualitative information that they typically are unable to communicate due to limitations in their linguistic capacity.
These tools help identify the character of pain (such as sharp or dull pain, soreness, stabbing, or throbbing pain) that clinicians rely on to make accurate diagnoses when children are unwell. They are tactile and offer a range of expressive possibilities, allowing young children to communicate qualitative information that they typically are unable to communicate due to limitations in their linguistic capacity.






Materials
Materials
Materials like metal, wood, ceramics, glass, and plastics are used in many medical device applications. Plastics have a wide range of desirable attributes that lend themselves to increased use in the design and development of many medical device applications. Complex shapes, multiple functionalities, and the use of a minimal number of parts (part reduction) in the device or product all make the use of plastics very attractive to designers. Such designs were not possible with materials like wood, metals, ceramics, and glass. Unique processing methods, assembly options, and design styles can reduce manufacturing costs.
Materials like metal, wood, ceramics, glass, and plastics are used in many medical device applications. Plastics have a wide range of desirable attributes that lend themselves to increased use in the design and development of many medical device applications. Complex shapes, multiple functionalities, and the use of a minimal number of parts (part reduction) in the device or product all make the use of plastics very attractive to designers. Such designs were not possible with materials like wood, metals, ceramics, and glass. Unique processing methods, assembly options, and design styles can reduce manufacturing costs.

